
Parenting Workshop
Join us for a supportive and interactive workshop exploring traditional parenting techniques, general parenting strategies, and ways to support grandparents raising grandchildren. 📅 Monday, March
Health Canada, First Nations, and Inuit Health criteria for eligibility to access the NIHB Program:
Registered First Nations individuals (Please Note: You must register your child with the Indian Registrar (DIAND) within the first year of birth, or they may not be eligible for NIHB Benefits after they turn 1 year of age)
The NIHB Program will cover the cost of benefits outside of Canada if you are attending school, employed or require approved medical treatment outside of Canada. The following items are covered as a benefit and include:
Private health insurance premium costs (for approved students, migrant workers and their legal dependents) will be reimbursed with proof of attendance at recognized institution or place of employment
Medical Transportation (for eligible clients when medically referred and approved by provincial or territorial health care plan) may be covered, click here for more information.
To ensure you are eligible for a benefit, and do not end up with out-of-pocket expenses for a service that was provided to you by one of the NIHB Service Providers, please ask the Service Provider if:
If you still have further concerns and/or questions in regards to your eligibility for a service provided under the Non-Insured Health Benefits please call the NIHB Client Information Line at: 1-800-640-0642; and for information on Dental: 1-888-283-8885.
The NIHB Drug Benefit List (DBL) provides a listing of the drugs eligible under the NIHB Program. This list in not an all inclusive list, your pharmacist will be able to provide you with what is covered under the NIHB benefits. Examples of covered drug benefits are:
IF YOU HAVE BEEN TO THE PHARMACY AND HAVE BEEN TOLD TO PAY AS THE DRUG IS NOT COVERED, PLEASE ASK THE PHARMACIST TO FORWARD THE PRESCRIPTION TO THE DRUG EXCEPTION CENTRE FOR PROCESSING.
This process has to take place before an appeal for coverage can be done.
The primary physician can send a request to the Ministry of Health and Long Term Care (MOHLTC) to cover the cost of the drug
The Ministry will review the request and let the physician know of the decision
The physician will then contact the client
For more information, click here.
The NIHB Dental Policy Framework (2005) and the NIHB Provider Guide for Dental Benefits (2009) define the terms, conditions, policies and benefits under which the NIHB Program will cover dental services. This is not an all inclusive list, your dentist will have a complete list.
For more information, click here.
All eye & vision care services requires prior approval to ensure client eligibility. Your eye & vision care provider will have a complete list. Examples of covered eye & vision care benefits are:
Other items that may be covered, but require medical justification include:
For more information, click here.
The ADP program is through the (MOHLTC) and is available to all Ontario residents ADP will cover up to 75% of cost for medical equipment and supplies.
The ADP and NIHB programs have eligibility criteria and guidelines that need to be followed. Once these criteria and guidelines are met the two programs will be utilized to best meet the needs of the individual. Your health care professional/service provider will have the complete list of criteria and guidelines and should coordinate benefits between the two programs to ensure that you have maximum coverage.
NIHB program will cover the 25% fee of eligible and approved NIHB items
Please Note: If the item is fully covered under a public/private health care plan, NIHB will not approve coordination of benefits, nor requests for co-payment to upgrade the quality of the item
For more information, click here.
or in the community of residence.
Long distance medical travel may include travel to the health services listed below.
(Prior approval is required through First Nations and Inuit Health):
Signed and dated confirmation of attendance and original receipts must be submitted for reimbursement.
In emergency situations, post approval may be granted (if consistent with the Framework)
For more information, click here.
Mental Health Professional must be an approved, registered provider with Health Canada
Prior approval is required (which will be submitted by your Mental Health Professional)
Up to 2 hours will be covered for the development of an assessment treatment plan
Approval for up to 15 one hour sessions (with a possible 5 hour maximum extension)
For more information, click here.
NIHB will fund clients up to a maximum of $150.00 per fiscal year (April 1 to March 31) for the chiropractic sessions
Please Note: The client is responsible for payment of the co-payment portion, previously known as the OHIP share (Average cost is $75.00 for an initial assessment and $45.00/ treatment)
For more information, click here.
When a client does pay directly for goods or service, they may seek reimbursement from the NIHB Program. Requests must be made on a Client Reimbursement Form, within one year from the date of service or date of purchase. Requests for reimbursement of eligible benefits must also include:
Click here for the Client Reimbursement Form.
EVERYONE HAS THE RIGHT TO APPEAL A DENIED BENEFIT!
When coverage for a benefit through the Non-Insured Health Benefits (NIHB) Program has been denied, the client or parent/guardian of the client has the right to appeal the decision
There are three levels of appeal available which only the client or parent/guardian can initiate. In order for a case to be reviewed as an appeal, a letter from the client or parent/guardian, accompanied by supporting information from the provider or prescriber must be submitted to the Non-Insured Health Benefits Program
APPEAL PROCESS for Dental, Eye & Vision Care, Medical Supplies & Equipment, Medical Transportation, and Short-term Crisis Intervention Mental Health Counselling
There are 3 levels of appeal under the NIHB Program:
Level I – Director NIHB / Ontario Region
Level II – Regional Director
Level III – Director General, NIHB
***Supporting and new medical documentation is required at each level.
There are 3 levels of appeal under the NIHB Program:
Level I – Director, Benefit Review Services
Level II – Director, Benefits Management
Level III – Director General, NIHB
***Supporting and new medical documentation is required at each level.
For more information, click here.

Join us for a supportive and interactive workshop exploring traditional parenting techniques, general parenting strategies, and ways to support grandparents raising grandchildren. 📅 Monday, March

UPDATE 2/25: This workshop is now FULL and a waitlist is being created. Contact Kelly to be added! Join us for a special two-day workshop

Accidental poisonings in children from edible cannabis can be life threatening. Store your cannabis out of reach and locked away. Suspect a poisoning? Call 1-844-POISON-X (1-800-463-5060
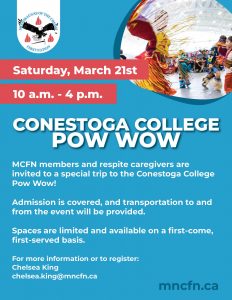
Open to MCFN members and respite caregivers – admission and transportation included! ⏰ Saturday, March 21st | 10 a.m. – 4 p.m. ⚡ Act fast –
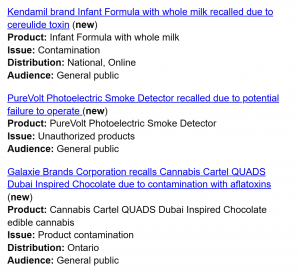
Community members are advised of the following recent recalls issued by the Government of Canada: • Kendamil Infant Formula (Whole Milk) – Recalled due to
